The safety and efficacy of medical devices are paramount, and microbiological testing can play a pivotal role in ensuring products are free from harmful microbes. Contamination can lead to serious repercussions, including infection and increased morbidity. Therefore, manufacturers cannot afford to overlook the stringent microbiological aspects of sterility testing. Here, we’ll guide you through what you need to know about microbiological testing as it relates to sterility testing, highlighting its significance and the associated regulatory landscape.
Understanding Microbiological Testing
Sterility testing is a critical phase in the approval process for single use medical devices, specifically those that come in contact directly with bodily tissues or fluids. The objective of microbiological testing within this context is to detect the presence of viable microorganisms. The test evaluates the bioburden (microbial contamination) left on the device after its manufacturing. Without data indicating the level of contamination, an appropriate cleaning and sterilization process for the device cannot be developed.
Why Microbiological Testing?
Microbial contamination of medical devices can occur during any stage of the manufacturing process, from component assembly to packaging. The presence of microorganisms on a device can lead to adverse reactions in patients, including infection, which can be life-threatening, particularly to those with compromised immune systems. Therefore, having in-depth knowledge of how devices can be processed to maintain their sterility at the microbial level is key to keeping patients safe.
Navigating the Regulatory Environment
Regulatory bodies such as the US Food and Drug Administration (FDA) and the European Medical Device Regulation (MDR) have stringent sterility testing standards that medical device manufacturers must adhere to. These regulations detail the types of testing required, acceptable microbial limits, and the need for validation of the testing methods used.
Compliance Is Non-Negotiable
To bring a medical device to market, manufacturers must rigorously demonstrate compliance with regulatory requirements. Failure to meet these standards can result in delayed approval, costly recall operations, and damage to the manufacturer’s reputation.
Microbiological Testing’s Vital Role in Patient Safety
The pursuit of patient safety is an underlying principle of microbiological testing in medical device sterility assessment. Pathogens are becoming increasingly resistant to antibiotics, making an already dangerous situation even more perilous. Rigorous microbiological testing is a good defense to prevent such occurrences.
Best Practices in Microbiological Testing
Routine microbiological testing in medical device manufacturing requires precision and attention to detail to ensure the test results are accurate and reliable. Here are some best practices to keep in mind.
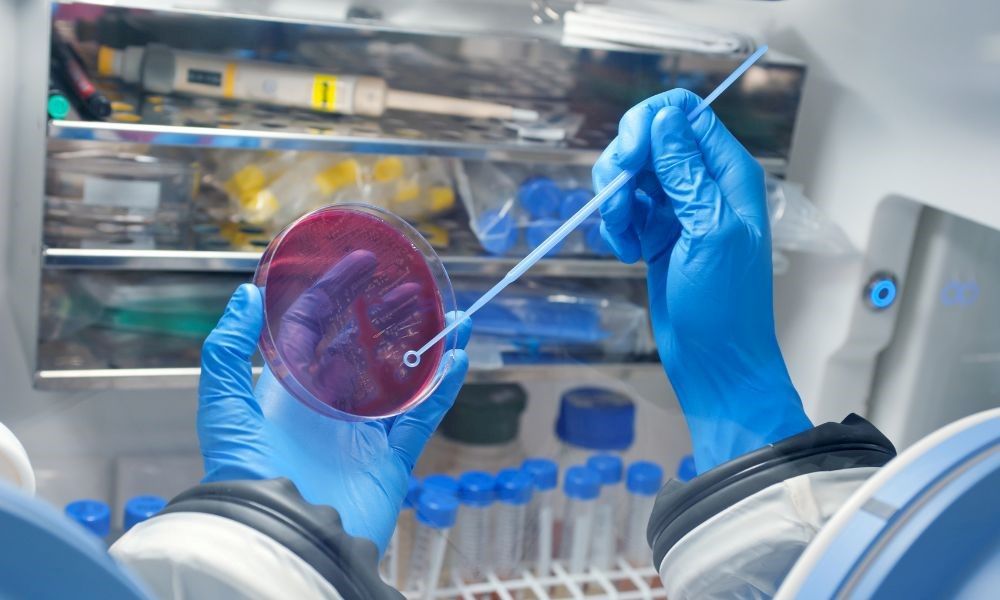
Sampling Techniques and Integrity
The sampling technique used to access devices is integral, as it directly affects the validity of the results. Proper sampling employs aseptic techniques to prevent cross-contamination and limit false positive results.
Method Validation and Quality Control
Utilizing validated testing methods is critical to obtaining consistent and accurate sterility results. Additionally, implementing robust quality control measures, such as ensuring the sterility of reagents and equipment, helps maintain the efficacy of the testing process.
The thoroughness of microbiological testing is a direct reflection of a manufacturer’s commitment to delivering safe and effective medical devices. By adhering to the highest standards of sterilization and conducting comprehensive testing, you protect patients and bolster your standing within the industry. Let HIGHPOWER help you with our comprehensive medical device sterility testing program. Our validation laboratory can perform thorough examinations of your products, ensuring they are safe to use from the moment healthcare professionals utilize them.