Medical device reprocessing is what makes reusable medical devices such as endoscopes, forceps, and other tools viable for use in health-care settings. Without adequate reprocessing procedures, these tools can transfer contaminants from patient to patient, increasing the risk of infection and putting patients’ health and safety at risk.
Reprocessing is more than a simple cleaning procedure, though. Both reusable medical device manufacturers and the health-care professionals responsible for cleaning and sterilizing these devices must understand the complexities of this procedure to ensure proper reprocessing between device uses. Learn more with this in-depth look at the reprocessing of reusable medical devices.
Factors That Influence Medical Device Reprocessing Procedures
Reusable medical device reprocessing is a detailed process that must account for factors such as the specific device, its usage, contamination risk, and clinical setting. These factors allow device manufacturers to create procedures that effectively clean and sterilize the device between uses, ensuring industry compliance and patient safety with every reprocessing procedure.
When developing reprocessing instructions for use (IFU), device manufacturers must also pay attention to the classification of the medical device. Reusable medical devices that have a higher risk of contamination require more thorough cleaning procedures.
Different Stages of Reprocessing
Though every reusable medical device has its own reprocessing procedure, there are always multiple steps involved. Below is an overview of those stages and the guidelines associated with them.
Point-of-Use Treatment
Reprocessing begins with point-of-use treatment. This refers to the initial steps that follow a surgical procedure or other contact with the patient. While at the point of use, health-care professionals must separate and remove any single-use or disposable items. Preventing soils from drying on instruments is also important, as dry contaminants are much harder to remove. Instrument transport gels or other products can keep devices moist until the cleaning process takes place.
Cleaning
After initial point-of-use treatment is the cleaning stage, where health-care professionals remove visible and invisible contaminants from the medical device. This thorough cleaning and rinsing process removes microorganisms from a device, but it is not meant to kill them the way disinfection or sterilization processes do. Instead, cleaning sets the foundation for these later stages of reprocessing.
In addition to prepping the device to allow for a more thorough and effective sterilization process, the cleaning stage helps prevent the spread of microorganisms. It also helps ensure the device is safe to handle during the rest of reprocessing.
The specific cleaning process for a reusable medical device varies based on the manufacturer’s IFU, the necessary level of microbial lethality, the device’s design and materials, and the intended use. It is crucial to select cleaning tools and products that align to these factors. Use detergents from the manufacturer’s IFU, change rinse water between uses, and only use purified water for a final rinse. Ensure that tools such as towels and brushes are clean and free of lint, soil, and other contaminants.
Inspection, Preparation, and Assembly of Instruments
After the reusable medical device is clean and dry, it undergoes inspection. The inspection process verifies that the device is clean before moving on to the next reprocessing stages. It also allows health-care professionals to spot any defects in the device and make necessary repairs or replacements.
The inspection and preparation process also works as a pre-check stage for sterilization. Health-care professionals should verify that the device is compatible with the upcoming sterilization cycle to prevent errors and damage.
They will also assemble and position the device to ensure the most effective pathway for the sterilization process to reach all surfaces of the device. This includes but is not limited to the following steps:
- opening lumen ports
- unlatching ratcheted instruments
- disassembling sliding pieces or removable parts
- placing the device in a way that concave or flat surfaces do not retain liquid during the sterilization process
Always follow the manufacturer’s IFU for proper preparation and placement ahead of sterilization.
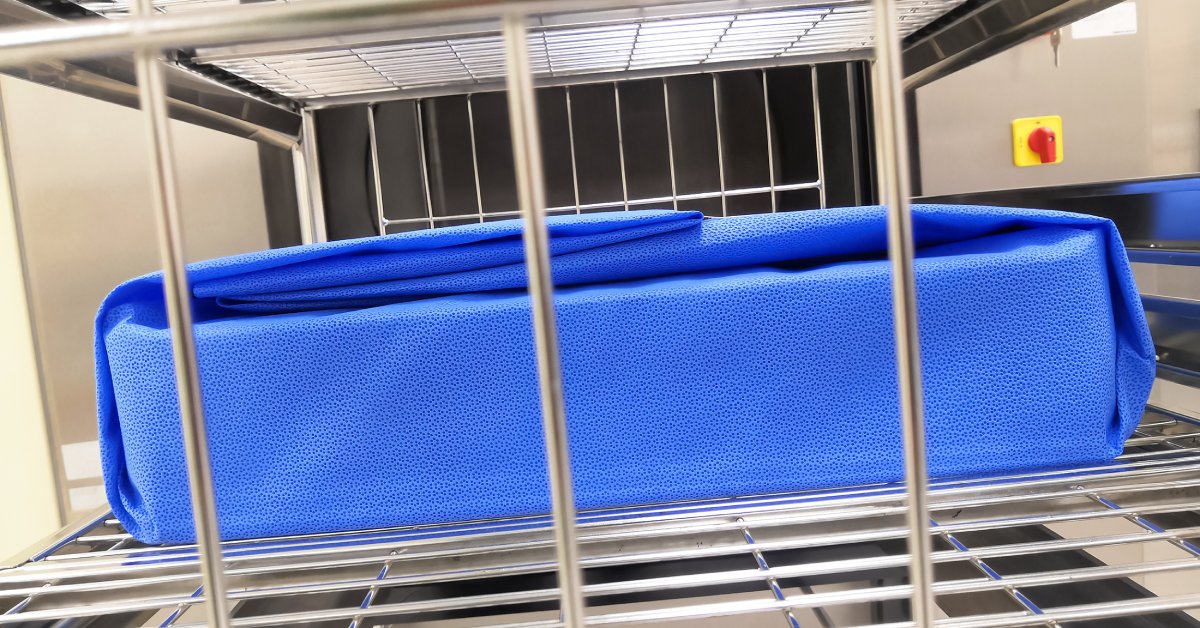
Packaging
The next step in reprocessing reusable medical devices is packaging. This is the final preparation before sterilization processes. Packaging protects the medical device and helps maintain sterility until it is ready for use again. This means that reusable medical device packaging designs must be durable enough to maintain the sterile barrier and keep the instrument intact while also allowing for sterilization processes to take place.
Health-care professionals prepare and package the device in wraps, pouches, or rigid containers to undergo sterilization. The manufacturer’s IFU will detail which sterile barrier systems to use for that device. The sterile barrier system must provide a barrier to microorganisms, resist tearing and puncture, create a tamper-evident seal, and allow for safe handling and opening without contaminating the device.
Labeling also plays a significant role. Packages require visible, legible labels made of nontoxic materials. The label cannot disrupt the sterile barrier or put the device at risk of contamination in any way. These labels should include the following information about the sterilization process:
- the sterilizer identifier
- the cycle and load number
- the date of sterilization
- a device description
- identifying information of the person in charge of device preparation and packaging
After packaging and labeling, the device is ready for the sterilization stage.
Sterilization
The specifics of the sterilization process depend on the type of reusable medical device you are handling. Common sterilization methods include steam sterilization and vaporized hydrogen peroxide sterilization. The manufacturer’s IFU will outline the sterilization procedure and include key information on sterilizer accessories, cycle parameters, load configuration, and other critical factors. Following these instructions ensures effective sterilization.
After the sterilization process, health-care professionals unload the device and perform an inspection to look for issues such as moisture or damage to the package. They should also note the package identification and mark any visual change to the external indicator. Careful handling and inspection play key roles in sterility assurance and ensure the reprocessing procedure is successful.
Sterile Storage
After sterilization, health-care professionals store the reusable medical devices until they are needed again. Responsible storage is necessary to maintain sterility and ensure the device does not become contaminated between reprocessing and reuse.
Guidelines for sterile storage include:
- keeping the device away from the floor, ceiling, and outside walls
- allowing for adequate ventilation
- keeping items safe from crushing, bending, or tearing
Only authorized personnel should have access to the sterile storage area.
Cleaning Validation With HIGHPOWER
A lot of work and research goes into developing and validating reprocessing procedures for reusable medical devices. Trust this process to the experts by turning to HIGHPOWER Labs for your devices’ cleaning validation tests. Learn more about our medical device decontamination services and validation processes by contacting our team today.